Day 1 :
Keynote Forum
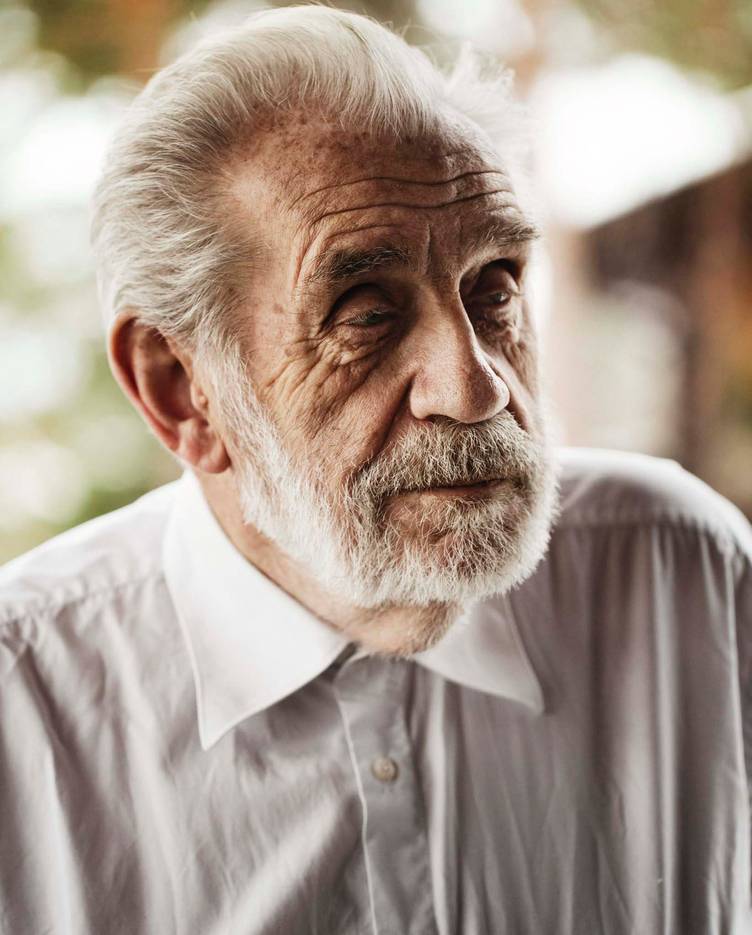
Akira Kaji
professor, University of Pennsylvania, USA
Keynote: The major action of Ribosome Recycling Factor (RRF) is to release mRNA from spent ribosomes—Use of this reaction for quick screening of specific antibiotic against RRF
Time : 09:45-10:30

Biography:
Akira Kaji has completed his PhD from The Johns Hopkins University followed by postdoctoral taining with Steven Kuffler at Johns Hopking Medical School follwed by Sidney Colowick at Vanderbuilt University, and David Novelli at OakRidge Natioanl Laboratory. He then became faculty member of University of Pennsylvania where he remains as an active professor. He has published more than 230 papers in reputed journals.
Abstract:
Protein synhesis has four steps, initiation, elongation of peptide chain, termination and the recycling of the spent ribosomes, mRNA and tRNA. The last step was discovered by our laboratories and catalyzed by a unique protein called ribosome recycling factor (RRF). The recycling step consists of three reactions, release of mRNA, tRNA and splitting of ribosomes. With the use of fluorescnt labeled mRNA similar to the natural mRNA and labeled tRNA, we demonstrate in vitro that the major action of RRF is to release of mRNA and not the splitting of ribosomes into subunits. This corrects the general misconcept that the major action of RRF is to split the ribosomes into subunits. The order of events with the naturally occuring substrate of RRF, the chain of events is release of tRNA, mRNA followed by the splitting of ribosomes. The release of mRNA is not dependent on the spliting of ribosomes. The in vitro results are supported by in vivo experiments where we used the tanlational coupling followed by the reporter gene expression (beta galactosidase expression). Using the basic reaction of RRF, release of ribosomes from mRNA, we developed a new screening system for the inhibitor of RRF. In this system, the inhibition of RRF reaction, makes ribosome stay on the mRNat the termination codon but start translating downstream which is linked to GFP. (222 words). We show that this screening method functions by the use of known specific inhibor of RRF, low concentration of fusidic acid. The assay method is simple and can be performed in 96 hole plate overnight. We look forward to find collaborators who has an access to the collection of possible inhibitors.
Keynote Forum
Y. Peter Di
Associate professor,University of Pittsburgh, USA
Keynote: Development of novel antimicrobials to overcome antibiotics resistance
Time : 9:40-10:20

Biography:
Dr. Y. Peter Di is an Associate professor in the Department of Environmental and Occupational Health, Director of Inhalation Exposure Facility, and Chair of Chemical and Hygiene Safety Committee at the University of Pittsburgh. His research focuses on the cellular and molecular actions of environmental or occupational exposures to toxic chemicals and microorganisms that underlie the pathogenesis of chronic human lung diseases including asthma, respiratory infection, COPD, and lung cancer. Dr. Di’s lab provided influential identification and characterization of a novel lung epithelial cell-specific secretory protein, SPLUNC1, and its roles in respiratory infection and pulmonary diseases. Dr. Di has contributed significantly to the recent development of natural and engineered antimicrobial peptides to overcome the multi-drug resistant (MDR) bacterial infection. Dr. Di’s laboratory studies the mechanisms of lung pathophysiology to provide a rational basis for the development of new approaches to treat pulmonary diseases.
Abstract:
Multidrug resistant (MDR) bacterial infections are linked to significant number of mortality and economic losses. The success of antibiotic development in the latter part of the 20th century led to a false sense of security that the medical field had achieved a sustainable control of infectious diseases, thus eliminating the perceived need for further development of novel antimicrobials. Unfortunately, the problem is worsening because of the void in the development and discovery of new antibiotics over the last three decades. We have previously developed a series of rationally engineered cationic antimicrobial peptides (AMPs) using different amino acids computationally arranged to achieve inactivation of diverse MDR bacterial strains. One of the lead engineered AMPs, WLBU2, has proven able to inactivate a broad spectrum of Gram-positive and Gram-negative bacteria in vitro at nM/μM concentrations, including MDR/XDR clinical strains of the ESKAPE pathogens. Importantly, WLBU2 has demonstrated efficacy in animal models of bacterial infection, including mouse models of P. aeruginosa bacteremia and a monkey model of vaginal Chlamydia trachomatis infection, demonstrating the ability of WLBU2 to work in complex biological environments intrinsic to animals. Furthermore, we evaluated the therapeutic potential of WLBU2 via direct airway delivery in a murine model of P. aeruginosa infection. With a single dose of 1µg (0.05mg/kg) delivered i.t., the initial effect of LL37 was moderate and transitory, as bacterial load and inflammatory cytokines increased at 24h with observed signs of disease such as lethargy and hypothermia, consistent with moribund state requiring euthanasia. In sharp contrast, WLBU2 reduced bacterial burden (>2 logs) and bacteria-induced inflammation (leucocytic infiltrates, cytokine and chemokine gene expression) at 6h and 24h post-exposure, with no observed signs of disease or host toxicity. To our knowledge, these studies represent the most successful published studies of in vivo testing of cationic AMPs in animal models.
Keynote Forum
Ghassan Matar
Professor and Vice Chairperson, American University of Beirut, Lebanon
Keynote: Combating antimicrobial resistance – Utility of antimicrobial combination therapy and/or inhibitors
Time : 11:20-12:00

Biography:
Dr. Ghassan M. Matar is a Professor and Vice Chairperson in the Department of Experimental Pathology, Immunology & Microbiology, American University of Beirut. To present he published 101 articles in refereed international journals and received funding from various extramural sources. His research interests deal mainly with molecular mechanisms of resistance to antimicrobial agents in pathogenic bacteria, namely carbapenem resistance in ESBL and non-ESBL producing Enterobacteriaceae and assessment of combination using antimicrobial therapy with and without inhibitors or natural products, in infections caused by carbapenem resistant Enterobacteriaceae harboring various carbapenemase encoding genes.
Abstract:
The range of antimicrobial agents that can be used to treat bacterial infections is becoming limited with the constant increase in antimicrobial resistance (AMR). Several genetic factors underlie AMR, including β-lactamase-encoding genes such as blaCTXM-15 that confers resistance to third-generation cephalosporins, and blaOXA-48, blaNDM-1, and blaKPC-2 that confer resistance to carbapenems. Remaining treatment approaches for such resistant infections include antimicrobial combination therapy and the use of β-lactamase inhibitors. This study assesses the molecular effects of such treatment approaches on antimicrobial resistant Enterobacteriaceae clinical isolates in vitro and in vivo.
Nine clinical Enterobacteriaceae isolates were included in the study. One harboring blaCTXM-15, one harboring blaOXA-48, one harboring blaKPC-2, two harboring blaNDM-1 and blaCTXM-15, and four harboring blaOXA-48 and blaCTXM-15. Minimal inhibitory concentrations were determined for carbapenems with β-lactamase inhibitors: avibactam, Ca-EDTA, and relebactam. Synergism between antibiotic combinations was determined by double disc diffusion when using colistin with several antibiotics. In vitro and in vivo gene expression levels were done on these combinations with and without inhibitors.
The use of meropenem, imipenem, and ertapenem with the selected β-lactamase inhibitors restored isolate susceptibility in 100%, 87.5%, and 25% of the cases, respectively. Antimicrobial synergism was mostly detected between colistin and meropenem, fosfomycin, or tigecycline. Survival studies revealed the survival of most mice receiving antimicrobial combination therapy with inhibitors as compared to the controls. Overall gene expression levels of resistance genes were variable depending on treatment.
The threat of antibiotic resistant bacterial infections remains viable; however, different approaches to therapy are available.
Keynote Forum
Helieh S. Oz
American Association o Gastroenterology
Keynote: Overuse of antibiotics in food animal industry and infectious and inflammatory complications in humans
Time : 12:00-13:00

Biography:
Workshop
Dr Helieh Oz has a DVM, MS (U. IL); PhD (U. MN) and clinical translational research certificate (U.KY). Dr Oz is an active member of American Association of Gastroenterology (AGA) and AGA Fellow (AGAF) and associate in Rome Foundation (Functional Gastrointestinal Diseases). Dr Oz is a Microbiologist with expertise in infectious and inflammatory diseases, drugs discovery, pathogenesis, innate/mucosal Immunity, molecular biology, and micronutrient. Dr. Oz has over 90 publications in the areas of chronic inflammatory disorders, microbial and infectious diseases. Dr Oz has served as Lead Editor for special issues including Gut inflammatory, infectious diseases and nutrition 2017 (Mediators of Inflammation); gastrointestinal inflammation, repair: role of microbiome, infection, nutrition (Gastroenterology Research Practice), J. Nutrient and guest Editor for J. Pediatric Infectious Disease. Dr Oz is a member of different editorial board and an avid reviewer for journals.
Abstract:
Pathogens cause dysregulated immune and inflammatory response. Microbiome in the gastrointestinal tract (GI) acts as a protector of health from disease. Microbiota helps absorption of nutrients and guards against invasive pathogens to dwell in GI. While, antibiotics are required to fight pathogens and infectious diseases, overuse and abuse as well as unintentional consumption of food contaminated with antibiotics affect GI to alter the composition of microbiome. Further, antibiotics shift equilibrium from health into disease status as in infections with Clostridium spp. Infectious protozoan and microbial diseases are transmitted from animals and cause GI inflammation and diarrhea in man. The common preventive practice for infectious diseases and growth promoter in farm animals are continued use (overuse) of antibiotics which enter blood circulation and contaminate eggs, milk, and meat products. Antibiotics are entered food chain and consumed by humans with possible allergic, antibiotic resistance, and other enigmatic side effects. It is estimated that over 80% of antimicrobials are used for prevention and growth promotion in swine, cattle and chickens compared to only 20% used in human therapies. This presentation will aim to discuss unintentional consumption of antibiotic residues in contaminated food products with possible side effects. Association between overuse and abuse of antibiotics in food animal industry will be discussed with outbreaks of major infectious foodborne diseases, altered gut microbiota and dysbiosis with serious complications. In addition, different preventive measures will be discussed including possible applications of new agents as surrogates to substitute antibiotics in food animals.
Keynote Forum
Rongshi Li
University of Nebraska Medical Center, USA
Keynote: Fragment-based and natural product-derived antibiotics against ESKAPE pathogens
Time : 09:00-09:45

Biography:
Abstract:
Keynote Forum
Tore Midtvedt
Karolinska Institutet, Sweden
Keynote: A holistic approach for evaluation of adverse effects regarding usage of antimicrobials
Time : 10:50-11:50
Biography:
Lecturer in Medical Microbiology, Department of Bacteriology,Faculty of Medicine, University of Oslo, Norway 1961-1963.Visiting scientist, Department of Germfree Research,Karolinska Institute, Stockholm, Sweden 1963-1966, Lecturer in Bacteriological Pharmacology.Faculty of Medicine, University of Oslo, Norway 1966-1969. Associated Professor in Medical Microbiology, University of Oslo 1973-1982. Professor in Medical Microbiology, University of Oslo, Norway 1982-1983. Professor and Chairman, Department of Medical Microbial Ecology,Cell and Molecular Biology, Karolinska Institute, Stockholm 1983-1999, Professor emeritus, Karolinska Institutet since 1990.Doctor Med Vet Honores Causae. Norw Sch Vet Med, Oslo Norway 2010.
Abstract:
In the present setting, the term eco-shadow is defined as future alterations in an ecosystem following exposure of the ecosystem to antimicrobial agens. The alterations can be of variable length and can involve variations in numbers and fuctions of species/strains as well as development of resistance to such agens.
In the past. most attention has been paid to development of antibiotic resistance following exposure of microorganisms to antibiotics. Nowadays. It is a rapid body of evidence showing that usage of any antimicrobial may lead to development of resistance and spreading of resistant microbial strains. Groups of substances studied to a certian degree include desinfectants, herbicides, pesticides, food additives, genetic modified organisms (GMOs)(dependiing of how they are produced), many heavy metals and even probiotics. Most often, the new resistance is found on plasmids, often rapidly coupled with resistance to commonly used antibiotics. Thus, usage of a desinfectant or a herbicide might be driving forces in a rapid spreading of resistance to clinically important antibiotics.
Therefore, our fight against increasing antibiotic resistance can not any longer be restricted to a more controlled usage of genuine antibiotics, but has to include a similar usage control of all antimicrobials. Additionally, new approches have to be taken into considerations Focus has to be put on spreading mechanisms. Cleansing of sewage will include eradication of antibiotic resistant genes, feces transplants have to be controlled for absence of defined gene resistance, etc, etc. This is not science fiction, but technologies under establishment.
Thus: eco-shadows following usage of any antimicrobial should be minimized
Keynote Forum
Rongshi Li
University of Nebraska Medical Center, USA
Keynote: Fragment-based and natural product-derived antibiotics against ESKAPE pathogens
Time : 09:00-09:45

Biography:
Abstract:
Keynote Forum
Akira Kaji
University of Pennsylvania, USA
Keynote: The major action of Ribosome Recycling Factor (RRF) is to release mRNA from spent ribosomes-Use of this reaction for quick screening of specifi c antibiotic against RRF
Time : 09:45-10:30

Biography:
Abstract:
Keynote Forum
Tore Midtvedt
Karolinska Institute, Sweden
Keynote: A holistic approach for evaluation of adverse effects regarding usage of antimicrobials
Time : 10:50-11:50

Biography:
Abstract:
Keynote Forum
John J S Cadwell
FiberCell Systems Inc., USA
Keynote: The hollow fi ber infection model: Principles and practice
Time : 11:50-12:35

Biography:
Abstract:
- Evolution and Mechanisms of Antibiotics and Antimicrobials Resistance | Antimicrobial Resistance and its Emergence of Animals | Antimicrobial Resistance: Emergence and its Eccentricity | Antibiotics: Types and Prognosis
Chair
Hideko Kaji
Thomas Jefferson University, USA
Session Introduction
Alessandro Pini
University of Siena, Italy
Title: The preclinical development of a novel antimicrobial peptide with strong antibacterial and anti-infl ammatory activity, systemic and pulmonary delivery with nanoparticles
Time : 12:35-13:00

Biography:
Abstract:
Nataliya Roth
University of Natural Resources and Life Sciences, Austria
Title: Role of feed additives in the strategy to reduce the prevalence of antimicrobial resistance in broilers
Time : 14:00-14:30

Biography:
Abstract:
Richard M Beteck
Rhodes University, South Africa
Title: Metronidazole Schiff base hybrids: Synthesis and in vitro anti-trichomonocidal evaluation
Time : 15:20-15:40

Biography:
Richard Mbi Beteck has completed his PhD from North-West University, Potchefstroom Campus and is currently a Postdoctoral Fellow at Rhodes University.
Abstract:
Hak-Ryul Kim
Kyungpook National University, Korea
Title: 7,10-epoxy octadeca 7,9-dienoic acid: Potential candidate for antibacterial agent against multidrugresistant Staphylococcus aureus
Time : 15:40-16:20

Biography:
Abstract:
Alessandro Pini
University of Siena, Italy
Title: The selective removal of LPS and LTA from human blood. Construction and use of a medical device based on the peptide SET-M33
Time : 16:20-16:40

